Dry Eye Center of Arizona
3805 E Bell Rd
Suite 1800
Phoenix, AZ 85032
CALL TODAY FOR AN APPOINTMENT
Phone (602) 549-2020
Fax: (602) 325-5536
dryeyecenter@gmail.com
Or use our contact form.
Office Hours
Our office is open during the following hours:
Mon-Friday: 9AM - 6PM
Doctor's Hours: By Appointment Only
LipiFlow Treatment
Dry Eye Therapy
Dry eye can rapidly become the bane of a patient's existence. Relief can be difficult to find and patients often travel from doctor to doctor seeking help. Today a number of different therapeutic approaches can target the specific cause or causes of your dry eye. They include:
Eye drops or artificial tears have long been an accepted therapy for dry eyes. Using drops would seem logical - add water to an eye that’s dry, dry eye disease is far more complex than just a lack of moisture. This is the primary reason simple drop formulations offer relatively little sustained benefit for patients and with too frequent application drops can actually cause harm by washing away or diluting important tear components.
Modern eye drops target specific dysfunction of the tears and tear structure. It is important to understand that drops for dry eye are not all the same.
Artificial tear drops can be divided into three main groups:
- Cushioning drops contain bulking agents - typically methylcellulose derivatives are designed to cushion the tears and action of the lids. Products like Allergan’s Refresh® and Optive® are popular and useful for some, however, these generally older formulations have been largely superseded my modern targeted formulations.
Advanced formulations include drops that mimic the function of tear components – in some cases nearly as effectively as natural tears. These include products like Alcon’s Systane® Ultra which mimics natural mucins to improve tear stability and viscoelasticity. AMO’s Blink® Tears contain hyaluronic acid which can help cushion and stabilize the tears. Several eyedrops act as lipid supplements. The best of these incorporate phospholipids which function as a bonding agent between the tear’s lipid outer layer and the underlying tear structure. Allergan's Refresh Mega-3 non-preserved drops, Alcon’s Systane® Complete and FreshKote® by EyeVance are the best of the lipid-based formulations. Note that FreshKote® may require an Rx.
Many artificial tears are available in both preserved and non-preserved unit dose versions. Modern preservatives have minimized the advantages of non-preserved drops for
most patients. Regardless, it is important to realize that while drops can be a helpful adjunct, they are never an effective treatment for dry eye - only a
temporary crutch.
Other over the counter eye products include a variety of gels, sprays and ointments. In general the gels are designed to afford greater protection for more severe dry eye or challenging environments. They last longer than comparable non-gel products. Ointments and sprays should be used after consultation with your doctor.
Because dry eyes are also sometimes red eyes, some patients are tempted to use drops aimed at reducing redness. Do not use drops intended to whiten the eyes. They typically contain ingredients that can worsen dry eye by disrupting the normal balance of the tears and irritating the ocular surface.
Modern advanced formulation drops provide far greater clinical performance than earlier products were able to. However, the many different products on the market and their complexity make it imperative that you seek professional advice to help you determine if drops will be of help and which drops will be of greatest benefit.
Nutritional Supplements and Dietary Considerations
Nutritional supplementation has become a well-accepted therapy for dry eye. Numerous studies have found that omega-3 fatty acids can containing supplements decrease dry eye symptoms, positively impact meibomian gland secretion, and also possess anti-inflammatory effects.
There are a variety of natural sources for omega-3s including cold-water fish, such as herring, sardines and salmon. Supplements containing fish oil are often
recommended. Flaxseed oil is reccomended but has little beneficial effect. PRN Dry Eye Benefits Omega-3 is our most frequent recommendation
as a product formulated specifically for dry eye. Some patients choose more common, but far less potent or effective Omega-3 supplements available from health food stores. Virtually all
"store brands" and heavily promoted products like Krill Oil do not reach therapeutic levels and are ineffective.
Many clinicians recommend that patients consume sufficient water. Dividing your body weight by 16 yields the recommended number of cups of water you should be consuming per day – although that
should be taken as a general recommendation. In general, consuming more water, but not excessive amounts of water can’t hurt and may help so its worth a try.
Medications for Dry Eye
Currently the only medications indicated and approved by the FDA for treating the signs and symptoms of dry eye in the United States are Novartis' Xiidra™, Sun's Cequa™, Kala's Eysuvis and OysterPoint's Tyrvaya™ Nasal Spray. Allergan’s RESTASIS® is approved for increasing tear production. Keep in mind that just a few years ago, no medications were approved for the treatment of dry eye disease. Many more medications are in development.
An ophthalmic emulsion containing the immunomodulator cyclosporine, Restasis® has been found to increase tear production in clinical trials. Restasis® is appropriate for some patients who have inflammatory dry eye. Clinical trials failed to demonstrate any increased tear production in patients who were using anti-inflammatory eye drops or had punctal plugs. Restasis® is taken twice daily and may take months or longer for any effect to be observed.
Cequa, introduced by Sun Pharmaceuticals, is another cyclosporine-based drop for dry eye. It contains double the concentration of cyclosporine and an advanced drug delivery system that makes it about four-times more potent than Restasis. In our experience, the medication works well for a large percentage of patients and is both comfortable and effective in managing chronic dry eye related inflammation.
Xiidra™ representeds a true breakthrough in dry eye treatment when it was introduced. The first medication approved by the US FDA for the treatment of both signs and symptoms of dry eye, this novel eyedrop was developed specifically for the eye by Shire, a global leader in pharmaceuticals. It is now owned and distributed by Novartis. Used twice daily and rapidly acting, most patients experience relief within days of starting this medication.
Xiidra™ safely and effectively blocks inflammatory T-cells cells from attaching to the eye's surface, thereby shutting down the inflammatory response that causes much of the misery of dry eye. With a close relationship with Shire during the development of Xiidra™ our experience has been nothing short of stellar. Many of our patients have experienced rapid and substantial relief including many who have failed with other treatments.
While all of the above medications may be an appropriate and effective treatment for many patients, dry eye is a complex, chronic and progressive condition. So, for some Xiidra™ or Cequa will be an important addition or adjunctive part of an overall long term therapeutic approach.
Topical steroid medications are often prescribed either alone or in conjunction with initiating Restasis® therapy. Dry eye is often accompanied by inflammation and steroids are the most effective way to squelch inflammation. However, steroids are not for long-term use as they have numerous potentially serious complications including glaucoma and cataracts. Steroids are typically used either for intermittent pulse therapy or for a limited time. A doctor must closely supervise steroid use.
Eysuvis from Kala pharmaceuticals is an advanced topical steroid anti-inflammatory that is approved by the US FDA for the signs and symptoms of dry eye. It is indicated for episodic use up to four times daily for up to two weeks at a time. It is especially safe when used as directed and is ideal for patients who suffer from dry eye flares where symptoms can suddntly worsen. It is not indicated for long term continuous use.
Tyrvaya is a recently introduced nasal spray that stimulates tear production through its action on the nasal trigeminal nerve. At this point, we don't view it as a first line treatment, but initial results suggest that it at least somewhat effective in 30% to 40% of patients. Because of the intensity of the response in some patients, it is not for everyone.
Antibiotics such as oral tetracycline class agents like doxycycline and topical drugs like azithromycin (Azasite®) are often used to help manage meibomian gland dysfunction. These drugs have effects that extend beyond their antibiotic indications including anti-inflammatory and lipid modifying properties. The use of steroid and antibiotic medications to treat dry is considered off-label as it is not approved by the US FDA, but both are commonly prescribed and well accepted medically.
There is good news on the near horizon with numerous new drugs to treat dry eye in the later phases of FDA investigation. Many of these novel medications appear to be promising and will broaden our ability to help patients.
Punctal Plugs
In healthy people, the rate of tear production, evaporation and drainage remain in good balance regardless of environmental or other challenges.
One strategy to retain more tears in the eye for longer involves restricting drainage using plugs that occlude the drainage system. Despite years of use, punctal plugs remain somewhat controversial. Some clinicians believe that tear stagnation and complications associated with plugs outweigh their benefits. With advances in pharmacologic management and recogniton of the role played by meibomian gland dysfunction in dry eye, use of punctal plugs has generally diminished, but they remain a viable although very rarely used option for some patients. A variety of different plugs that either fully block or restrict tear drainage can be inserted in a quick, painless in-office procedure.
Punctal cautery is a permanent form of punctal occlusion which we caution patients to avoid. In many cases, we need to remove punctal plugs that are causing problems. Punctal cautery cannot be reversed without invasive surgery.
Lid Hygiene
Healthy lids are critical to managing dry eye and ocular surface disease. The lids contain the critically important meibomian glands which help support a healthy and stable tear structure. Bacterial overpopulation of the lids is extremely common and requires aggressive management.
Hyclear by Contamac has rapidly become a mainstay therapy for patients with dry eye and meibomian gland dysfunction. It is also used to treat blepharitis, an inflammation of the lids and lashes. Consisting of pure stablized hypochlorous acid, the same agent that white blood cells use to neutralize infection, Hyclear not only reduces bacterial overpopulation, it also inactivates bacterial toxins and blocks enzymes that can attack the protective lipid layer and destabilize the tears. In most cases, Hyclear is applied directly to the closed eyelids morning and night.
It is important to note that there are several hypochlorous acid "knock-offs" that contain significant amounts of toxic laundry bleach. For that reason, it is important to insist on Hyclear brand which is pure hypochlorous acid.
Treatment for meibomian gland dysfunction (MGD)
There has been a veritable renaissance of thinking regarding dry eye in recent years. MGD has increasingly been recognized as a primary cause of dry eye disease. Treatment for MGD has typically consisted of warm compresses performed at home with lid massage to express the meibomian glands. In office treatment has centered around manually expressing the meibomian glands to clear blockage. These approaches are still performed, however, new research has suggested that vigorous massage of the eyes after warm compresses can cause permanent distortion and negatively impact vision so this is no longer recommended. Office gland expression remains a helpful technique, but usually needs to be repeated frequently and can be uncomfortable.
An important step in treating meibomian gland dysfunction is debriding - or removing the excessive buildup of cells, debris and biofilm from the area around the meibomian glands - called Marx's line. This helps unblock the glands. The recently introduced BlephEx device is a gentle but extremely effective way of debriding the lid margins. We perform this procedure typically every six months.
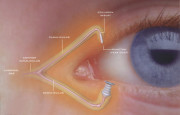
TearScience, a division of Johnson & Johnson, produces the LipiFlow® and LipiView® devices for treating MGD. We are remain among a small number of practices in the US to incorporate this innovative technloogy. The LipiView® provides a detailed view of the tear film using interferometry which permits precise measurement of lipid layer thickness down to nanometer levels.
The LipiFlow® device provides vectored thermal pulsation to warm the meibomian glands through the inside of the lids and gently massage thickened meibum (lipid) and debris from the gland. This system is cleared by the US FDA for the treatment of MGD and evaporative dry eye. With hundreds of patients successfully treated in our center, LipiFlow® has proven to be safe and effective.
TearCare® by Sight Sciences is a novel treatment option for MGD using externally applied computer controlled heat. We were the very first practice in the United States to add this technology to our treatment options for meibomian gland dysfunction. It is the only fully open eye procedure for MGD and allows for precise and customized treatment of obstructed meibomian glands for our patients.
iLux® by Alcon is another in a growing field of FDA cleared treatment options for MGD. It is an advanced assisted treatment technology that allows for controlled delivery of heat and force-limited pressure to the lids to express obstructed meibomian glands. Its LCD display provides constant data on treatment parameters. iLux is expecially useful for targeted gland expression and is a comfortable and effective choice for many patients.
IPL or Intense Pulsed Light therapy initially derives from dermatology where it has been used for several decades to treat a variery of conditions including facial rosacea, vascular and pigmented skin lesions. as well as for skin rejuvination. More recently, IPL has been shown to be extremely effective for managing meibomian gland dysfunction, dry eye and ocular forms of rosacea. It was approved by the US FDA for the management of dry eye in 2021 and the new Lumenis OptiLight System introduced. We utilize a state-of-the-art Lumenis Optima® M22 and the Lumenis OptiLight IPL which is considered a standard of care device for dry eye and MGD treatment. Treatment is typically accomplished in 4 sessions scheduled approximately 3 to 4 weeks apart. IPL is applied to the skin surrounding the eyes which are protected by special shields. In some cases the eyelids care treated directly. Sessions last about 10 to 15 minutes and are quite comfortable.
IPL is thought to work by sealing abnormal blood vessels that leak inflammatory elements into the ocular tissues. Other effects observed include improved meibomian gland function, and improved tear stablity and patient comfort. Results are usually seen by the second or third treatment and have been extremely impressive for the majority of patients. Retreatments may be performed in six months to a year if necessary.
Additional treatments for MGD include probing which is thought to open sealed glands, but is somewhat controversial due to possible inadvertent damage to gland structures. We avoid gland probing as potential risks and complications outweigh benefits.
More informaton on dry eye can be found in the sections on The Normal Tear Film, What is Dry Eye?, Diagnosing Dry Eye, and Dry Eye Therapy.